A space and place for women’s wellness.
We are a full service integrative women's health practice located in Winston Salem, North Carolina. We were built on filling the gap in women’s health we observed in traditional medical model, and we are fierce advocates for evidenced based, compassionate care.
Our approach
Camel City Women’s Wellness is an integrative women’s health practice that serves women across the lifespan. We provide trauma informed care with solution focused treatment plans. We focus on educating, empowering, and delivering evidence based high quality medical care to our patients, by placing high value on continuing education, medical research and technologies, community engagement, and compassionate care of our patients.
Providing you with a safe space to tap into your health and wellness.
All your appointments will take place in our soothing office environment with low lighting, private rooms, and by compassionate, trauma-informed people.
Winston-Salem office conveniently located off Interstate 40.
In-person and remote options
Our office is conveniently located off Healy Dr. in Winston Salem, NC. We also offer telehealth options for all individuals who reside in North Carolina.
Our services
-

Hormone Health
-

Preventative Health & Lifestyle Medicine
-

Sex Medicine
Meet our team
-

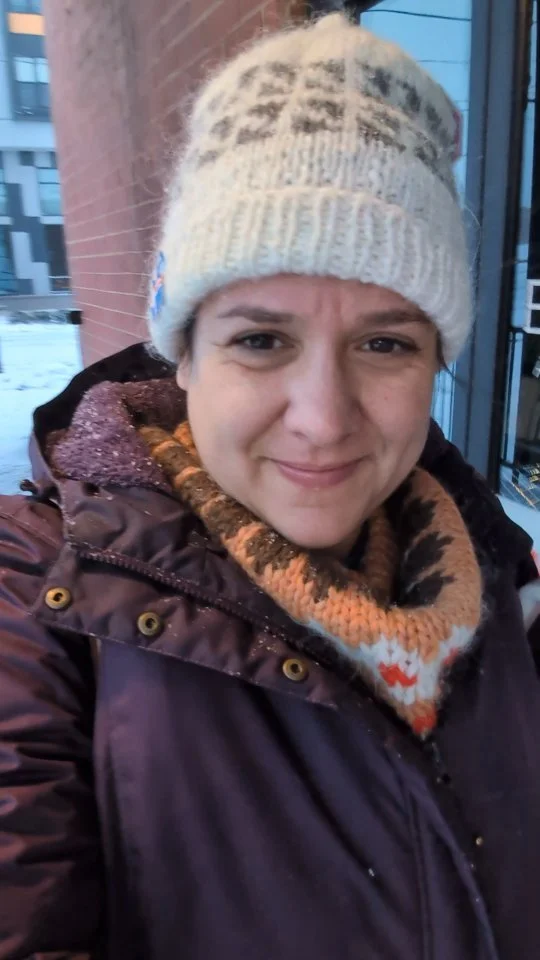
Christina Saldanha, PA-C
-

Mikel Getz - Patient Care Coordinator
“When I came to Camel Women's Wellness I had a myriad of symptoms related to menopause; hot flashes, weight gain, fatigue, irritability, all of it. I had talked with my Gyno, my GP, and an integrative MD. No one could give me an optimistic outlook, I was just going to have to deal with it. Christina was able to help me not just understand what was truly happening with my body, but also give me a clear path to addressing the symptoms. I feel light years better, genuinely more myself. I wasn't alone in this, and I am forever grateful.”
— PATIENT